Internal Medicine
Our Program
The Northwest Health – Porter Internal Medicine Residency Program is a three-year program Accredited by the ACGME and participating annually in the NRMP Match.
Our program’s mission is to train physicians to become excellent internists capable of utilizing a strong foundation of both inpatient and outpatient medicine to succeed in the career path they choose. We aim to live this mission by:
- Providing dedicated clinical experiences with sufficient durations that fully immerse residents in the educational experience, promote and foster professional rapport and feedback opportunities with supervising faculty, and increase continuity of care for the patients we serve
- Creating strong internists who will excel in today’s healthcare environment through a careful balance of inpatient and outpatient medicine
- Integrating rural, community medicine into the program’s foundation through required experiences in a rural, critical access hospital (Northwest Health – Starke) to respond to the unique needs of our community
- Demonstrating responsiveness to and mentorship of each resident so they feel capable of and empowered to pursue any field of medicine they desire
Academics
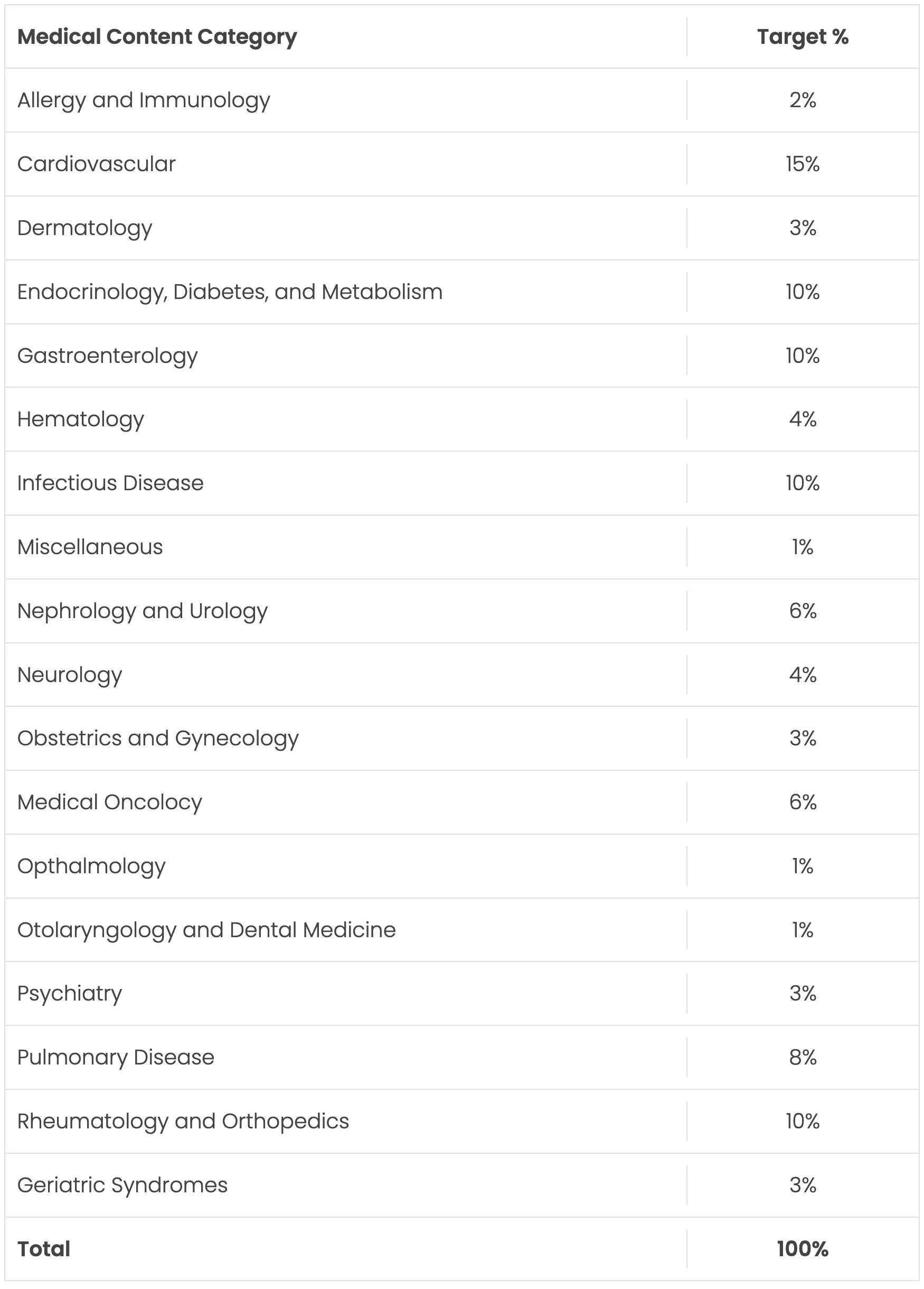
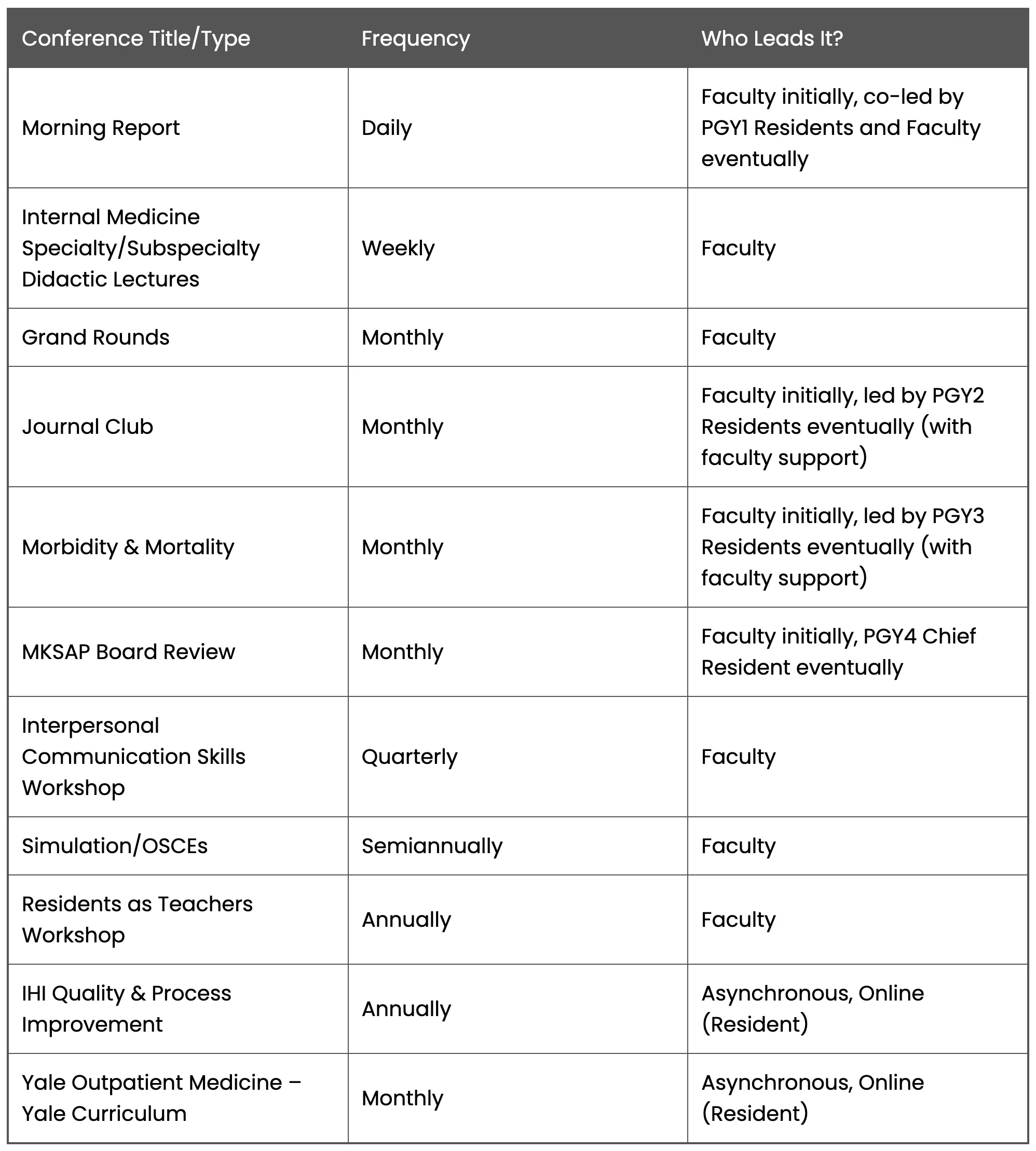
Instead of daily noon conference, residents attend a weekly didactic half-day the structure of which includes a balance of topics and presenter mix, resident v. faculty. Topics will be balanced in proportion to the ABIM’s Blue Print to the Board Exam. The ABIM Blue Print allows the program the ability to assure the specialty-specific lectures along an 18-month recurring curriculum provide the highest probability of assuring the educational needs of residents are met for board prep.
In addition to these topics, lectures will be given on social determinants of health, quality and process improvement, business of medicine, medical ethics, diversity and inclusion, and other subjects determined necessary and relevant by the Program Evaluation Committee.
Didactics will be in-person, onsite at Northwest Health – Porter on Thursday mornings from 7am to 1pm. Residents unable to attend can join virtually via GoogleMeet. The didactics are structured with a weekly “theme” based on ACGME-required learning (quality/process improvement, addiction medicine, etc.) and ABIM Board Exam Blue Print (Cardiology, Endocrinology, etc.). Material related to all conferences such as journal articles, presentation material, and handouts will be stored in New Innovations under the Conference Module. Residents need only log in, navigate to the conference schedule and click the conference of interest to access, download, and review the knowledge content they missed. Faculty can also use this to download their lecture from 18 months ago when the curriculum repeats so all they have to do is update it with any new evidence-based practices.
More Information on Didactics:
Morning Report, Daily, 7:00-8:00 AM: Occurs Monday through Friday at Northwest Health – Porter and includes supervised sign-out and the residents will present a 20-25 minute inpatient based case-based topic that demonstrates key aspects of either diagnostic/therapeutic issues encountered on their patients. PGY1s on the Inpatient Medicine service are responsible for selection of case presentations at Morning Report. These presentations should be evidenced-based, review high value care diagnostic and therapeutic decision making, and preferably involve the specialty education of the week.
Morbidity & Mortality or “M&M”, Monthly on Wednesday AMs: A clinical teaching faculty will be paired with 1-2 residents to select, review, and lead discussion on a deidentified patient case for quality or patient safety issues, opportunities, and systems-based prevent measures that can be deployed to prevent a negative outcome in the future for similar cases. PGY3 residents will be required to lead at least one M&M.
Journal Club, Monthly on Wednesday AMs: A clinical teaching faculty will be paired with 1-2 residents to select, critically appraise, and lead discussion on a journal article. Discussion will include the applicability of the study to current evidence-based and cost-effective practices, and the ability to apply the study to patient care in everyday practice as relevant. PGY2 residents will be required to lead at least one Journal Club.
Observed Structured Clinical Exams (OSCEs): Residents will participate during orientation so the program can observe and understand competency levels for Interpersonal and Communication skills at the residents’ initial appointment into the program. The OSCE results will then become the benchmark for continued improvement and growth during each subsequent six-months of training. OSCEs will continue annually so the program can gauge the efficacy of these communication workshops as well as monitor and guide residents’ progress toward competency in each of the three Interpersonal Communication Skills sub-competencies.
Communication-Oriented Workshops: Provided periodically throughout training and will focus on teaching important skills such as communication methods which support the development of therapeutic, professional relationships with patients and their families, acting as a patient advocate with other entities in the greater health system, and effective communication practices for maintaining a healthy work culture in a team-based care setting.
Scholarly Activity
The program requires that residents complete at least two scholarly activity projects by the end of training. This requirement and methods for satisfying it will be provided at Initial Appointment orientation. For example, PGY2 residents will be required to lead at least one Journal Club. PGY3 residents will be required to lead at least one Morbidity and Mortality conference. Residents will be encouraged and supported, however, in going above and beyond these minimum requirements. Residents whose work is accepted for poster or oral presentation will have up to $3,000 of the costs covered for conference attendance. Residents whose work is accepted for publication can request and may be granted additional administrative time to work on revisions so as to assure success in publication.
Clinical Training Curriculum
Instead of structuring clinical training rotations changing every month with a half-day of continuity clinic (e.g., outpatient medicine curriculum) weekly, our program is taking a progressive approach, called an “X+Y Model.” The X+Y works within the constraints of the specialty-specific requirements to separate out the continuity clinic/outpatient medicine curriculum so that residents can be fully immersed in each rotational assignment. It allows, for example, a resident to work in the ICU for four weeks straight and never have to leave their critically ill patients to see patients in the clinic. Following those four weeks, they transition to the continuity clinic to begin a two-week rotation in outpatient medicine.
This 4+2 clinical training model thus provides a balanced approach to training well-rounded physicians in the field of Internal Medicine and its subspecialties.
Inpatient (Months)
Location: Mostly at Northwest-Porter unless otherwise stated.
- PGY-1: 6 months = 4 months Inpatient Medicine, 1 month ICU, 1 month at Northwest Health – Starke
- PGY-2: 4 months = 2 months Inpatient Medicine, 1 month of Nights as 2-week blocks, and 1 month ICU
- PGY-3: 4 months = 2 months Inpatient Medicine, 1 month of Nights as 2-week blocks, and 1 month of ICU
Outpatient (Months)
Location: Portage of Valparaiso Clinic, depending on resident assignment.
- PGY-1: 4.5 months = Outpatient Medicine as 2-week blocks after 4-weeks of other experiences
- PGY-2: 4.5 months = Outpatient Medicine as 2-week blocks after 4-weeks of other experiences
- PGY-3: 4.5 months = Outpatient Medicine as 2-week blocks after 4-weeks of other experiences
Putting it all Together
A summary of the full clinical training experience our graduates will enjoy over three years is noted below:
- Inpatient (Hospital) Medicine – 8 Months
- Night Float – 2 Months
- Critical Care Medicine – 3 Months
- Outpatient Medicine – 13 Months
- Cardiology – 2 Month
- Gastroenterology – 1 Month
- Hematology/Medical Oncology – 1 Month
- Pulmonary Medicine – 1 Month
- Individualized Educational Experiences (Electives) – 6 Months
Electives include all Internal Medicine subspecialties, Rural Health at Northwest Health – Starke, Emergency Medicine, Neurology, Women’s Health, Psychiatry/Behavioral Health, Underserved Medicine (Free Clinic or an FQHC), Quality and Process Improvement, and Research. Residents may also request “designer” rotations for the Program Director to consider and approve as appropriate for the educational needs and career interests of the resident.
All residents enjoy four-weeks of vacation/paid time off during each academic year of training.